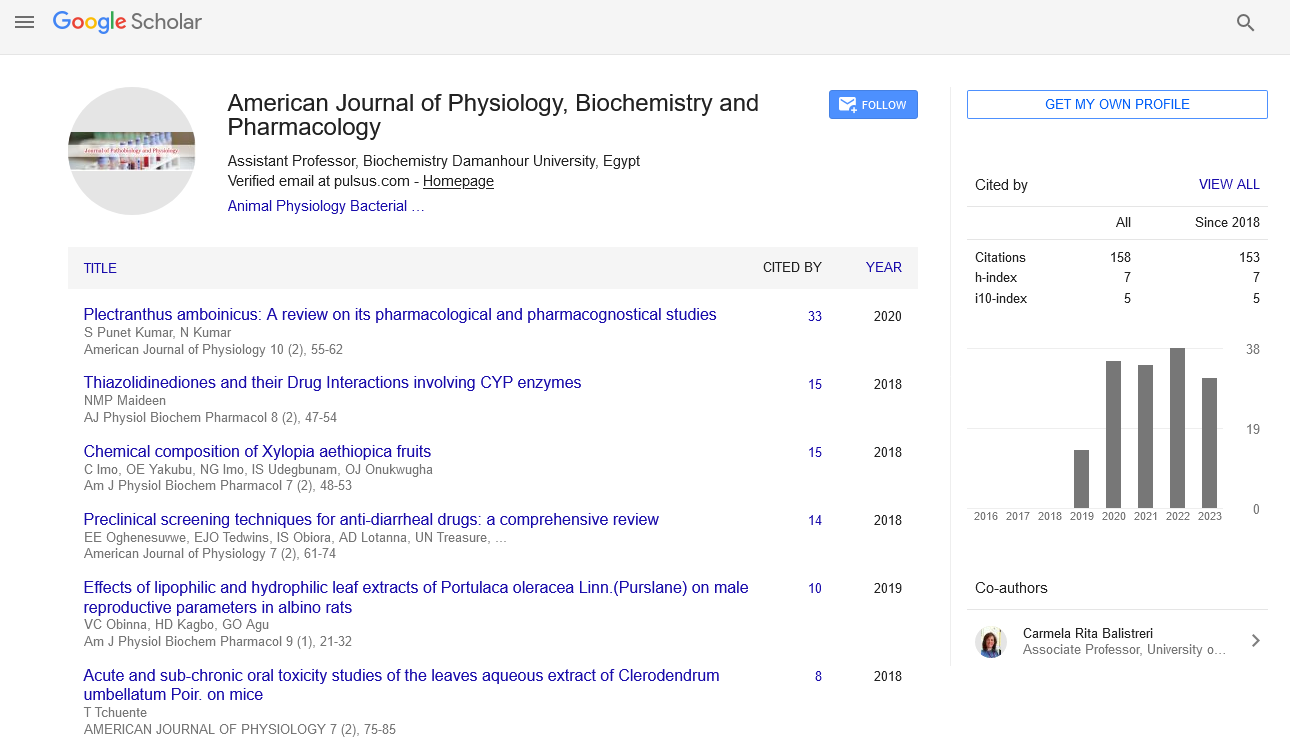
Opinion Article - American Journal of Physiology, Biochemistry and Pharmacology (2023)
The Impact of Blood Pressure on Cardio-Metabolic Risk Factors
Ferne Rosser*Ferne Rosser, Department of Pharmacology, The University of Jordan, Amman, Jordan, Email: rosserferne@gmail.com
Received: 26-Sep-2023, Manuscript No. AJPBP-23-121140; Editor assigned: 29-Sep-2023, Pre QC No. AJPBP-23-121140 (PQ); Reviewed: 13-Oct-2023, QC No. AJPBP-23-121140; Revised: 20-Oct-2023, Manuscript No. AJPBP-23-121140 (R); Published: 27-Oct-2023
Description
Cardio metabolic diseases, a cluster of disorders encompassing cardiovascular diseases, metabolic syndrome, and diabetes, have emerged as a significant global health concern. Among the key factors contributing to this epidemic is the intricate interplay between blood pressure and cardio metabolic health. Understanding the dynamic relationship between these two elements is crucial for unraveling the complexities of cardiovascular health and devising effective preventive and therapeutic strategies.
Blood pressure dynamics
Blood pressure, the force exerted by circulating blood against the walls of arteries, is a vital physiological parameter. It is typically measured in millimeters of mercury (mmHg) and consists of two components systolic pressure, representing the force during heartbeats, and diastolic pressure, denoting the pressure when the heart is at rest between beats. The standard measurement is expressed as systolic over diastolic pressure (e.g., 120/80 mmHg).
Cardio metabolic disease overview
Cardio metabolic diseases encompass a spectrum of conditions that affect the heart and metabolic processes. Cardiovascular diseases, such as coronary artery disease and stroke, are major components, alongside metabolic syndrome and diabetes. Metabolic syndrome is characterized by a cluster of interconnected factors, including abdominal obesity, high blood pressure, elevated blood sugar levels, and abnormal lipid profiles.
Diabetes, on the other hand, is a chronic condition marked by elevated blood sugar levels, leading to complications affecting various organs, including the heart.
The interconnection between blood pressure and cardiovascular diseases
Hypertension as a cardiovascular risk factor: Elevated blood pressure is a well-established risk factor for cardiovascular diseases. Persistent high blood pressure can damage the arteries, leading to atherosclerosis, a condition where plaque builds up, narrowing and hardening the arteries. This process increases the workload on the heart, raising the risk of heart attacks, strokes, and other cardiovascular events.
The bidirectional relationship: The relationship between blood pressure and cardio metabolic diseases is bidirectional. Not only does high blood pressure contribute to cardio metabolic disorders, but these conditions can also exacerbate hypertension. Insulin resistance, a hallmark of metabolic syndrome and type 2 diabetes, may contribute to the development of hypertension. Additionally, obesity, a common feature of metabolic syndrome, can lead to increased blood volume and cardiac output, contributing to elevated blood pressure.
Endothelial dysfunction: Endothelial cells lining blood vessels play a crucial role in regulating blood pressure. Dysfunctional endothelium is a common feature in both hypertension and cardio metabolic diseases. In conditions like diabetes, chronic inflammation and oxidative stress can impair endothelial function, contributing to elevated blood pressure. Conversely, hypertension can exacerbate endothelial dysfunction, creating a vicious cycle that promotes cardiovascular complications.
Insulin resistance and blood pressure: Insulin resistance, a key factor in metabolic syndrome, can directly impact blood pressure regulation. Insulin promotes sodium reabsorption in the kidneys, leading to increased fluid retention and elevated blood pressure. Furthermore, insulin resistance is associated with sympathetic nervous system over activity, which can contribute to increased heart rate and blood vessel constriction, both raising blood pressure.
Obesity as a common denominator: Obesity, a shared risk factor for both hypertension and cardio metabolic diseases, significantly influences the relationship between blood pressure and metabolic health. Adipose tissue secretes various bioactive substances, including inflammatory cytokines and adipokines, which can contribute to insulin resistance, endothelial dysfunction, and elevated blood pressure.
The intricate relationship between blood pressure and cardio metabolic diseases underscores the need for a holistic approach to cardiovascular health. Targeting one aspect without considering the broader interconnections may provide only partial benefits. Lifestyle modifications, including a balanced diet, regular physical activity, and weight management, play a pivotal role in preventing and managing both hypertension and cardio metabolic disorders.
Moreover, early detection and intervention are paramount. Routine blood pressure monitoring and regular health check-ups can help identify individuals at risk, enabling timely interventions to mitigate the progression of cardio metabolic diseases. Research into pharmacological interventions that target shared pathways in blood pressure regulation and metabolic health holds promise for future therapeutic strategies.