Mini Review - American Journal of Physiology, Biochemistry and Pharmacology (2024)
Therapeutic Response Monitoring: Minimal Residual Disease Testing in Cancer Management
Shu-Ju Ahn and Chen Yuguang*Chen Yuguang, Independent Researcher, OncoDxRx, LLC, Los Angeles, USA, Email: cyeh.oncodxrx@gmail.com
Received: 17-Oct-2024, Manuscript No. AJPBP-24-150550; Editor assigned: 21-Oct-2024, Pre QC No. AJPBP-24-150550 (PQ); Reviewed: 04-Nov-2024, QC No. AJPBP-24-150550; Revised: 12-Nov-2024, Manuscript No. AJPBP-24-150550 (R); Published: 20-Nov-2024
Abstract
Clinicians are tasked with monitoring drug treatment effects to ensure safe and effective therapy. While monitoring response to treatment is vital in cancer management, reliable biomarkers for non-invasive, longitudinal, and real-time evaluations are still challenging to find. Often, monitoring is done inappropriately—too much, too little, or at the wrong time-and isn’t always targeted at clinically useful parameters. Moreover, monitoring involves more than objective laboratory tests; it requires patient participation through reporting clinical response signals.
Innovative cancer research is focused on identifying biomarkers with diagnostic, prognostic, predictive, and therapeutic value. Developing accurate and robust cancer biomarkers is important for precision diagnostics and personalized treatment. These biomarkers should be used to assess therapeutic intervention efficiency, allowing early detection of therapy response, treatment failure, and disease progression or relapse. Detailed on-treatment biomarker monitoring is essential for personalized medicine. This article reviews some principles of minimal residual disease testing for therapeutic response monitoring, aiming to enhance benefits, reduce adverse events, and lower costs.
Keywords
Cancer; Biomarker; Therapeutic response monitoring; Minimal residual disease; Testing
Introduction
Cancer remains a leading cause of death. Its incidence will continue to rise with increasing global life expectancy, adding pressure to already fragile healthcare systems. While scientific and medical advances have dramatically improved approaches to cancer treatment, recurrence remains a significant concern. Investigators need a highly sensitive method to detect the slightest trace of residual disease, which, if left undetected, could lead to a drug-resistant relapse.
Cancer therapy has dramatically improved in recent years, to the point that individuals with certain disease types experience remission with relative frequency. Given this increasing rate of success, there is now greater focus on measuring and monitoring the remaining cancer cells following successful treatment. Often referred to as minimal or Molecular Residual Disease (MRD), the presence and relative quantity of these cells can indicate whether a patient has achieved a sustained deep molecular response. Such an indication could mean the patient is eligible to reduce or cease treatment with minimal fear of recurrence.
Accurately detecting and quantifying MRD can be challenging. Model imaging and tissue pathology technologies cannot resolve small numbers of cells, limiting their capabilities to effectively detect changes in tumour status, including recurrence. Fortunately, liquid biopsies offer a solution for rapid, cost-effective, and minimally invasive serialized analyses. When paired with a highly sensitive platform for precisely detecting levels of mutation markers, this diagnostic method could provide critical information used to guide therapeutic steps when treating relapse. Today, scientists can detect MRD by identifying circulating tumour DNA (ctDNA) shed into the blood by tumour tissue, but many molecular technologies, such as widely adopted Next-Generation Sequencing (NGS), are not sensitive enough to reliably measure the presence of MRD. In fact, data suggests measurable MRD is below NGS’s limit of detection approximately half the time. Recent studies demonstrate that an alternative to NGS called droplet digital PCR (ddPCR) is more sensitive [1]. As such, it is capable of robustly detecting low abundance nucleic acid in liquid biopsies while also providing critical information about absolute quantification of mutated DNA. Such data can be used to provide a clearer understanding of a patient’s need for ongoing treatment and risk of recurrence.
Literature Review
Optimizing biomarker tracking
Growing evidence demonstrates the value of MRD as a prognostic marker across a variety of cancer types. However, scientists must identify relevant targets to distinguish the small amount of mutated DNA within liquid biopsies. Scientists have established many “standard” biomarkers for certain cancer types due to how frequently they occur: for example, EGFR for metastatic lung cancer; KRAS for colorectal, lung, and pancreatic cancer; BRAF and NRAS for metastatic melanoma; and BCR-ABL1 for Chronic Myeloid Leukaemia (CML) [2-5]. Yet a variety of mutations can lead to a single type of cancer and, therefore, it has become common practice to sequence a patient’s tumour to find multiple biomarkers to track through serial liquid biopsies.
Monitoring relapse
In the case of CML, MRD testing is a well-established component of a patient’s journey, as it can indicate when it is safe for patients to discontinue treatment with Tyrosine Kinase Inhibitors (TKIs). TKIs have been therapeutically transformative for individuals with CML, granting them a relatively normal life expectancy. However, these drugs are costly and can limit a patient’s quality of life due to a number of side effects. Accurate and sensitive MRD testing can indicate a safe cut-off for TKI treatment, saving patients from years of expensive treatments and debilitating side effects.
Demonstrating the value of increased testing sensitivity, investigators performed MRD analysis on 172 CML patients in the largest US-based study of its kind. Individuals had achieved a major molecular response (i.e., BCR-ABL1 transcript levels below 0.01 percent for at least two years) via TKIs, indicating they were eligible to stop treatment. After discontinuation, the team monitored MRD levels using ddPCR and qPCR. qPCR detected MRD in 28 patients, and half of them relapsed. DdPCR technology detected an additional 56 patients who harboured MRD that qPCR did not detect, and 36 of these patients (64.3%) relapsed. Meanwhile, in 87 patients, neither qPCR nor ddPCR detected MRD, while only nine of these patients (10.3%) relapsed [5].
Similarly, due to the technology’s limits of sensitivity, qPCR often cannot inform clinical decision-making in patients with Mantle Cell Leukaemia (MCL). In one study, ddPCR outperformed both qPCR and flow cytometry for detecting MRD at low variant allele frequencies of 0.01-0.001. The authors proposed guidelines for using ddPCR to evaluate MRD in MCL cases [1].
The use of MRD testing continues to grow for solid tumour cancers. For example, in a study of 150 patients, researchers profiled tumors using NGS and then tracked two genetic biomarkers using ddPCR. Following surgery, the researchers found that the presence of MRD, as measured using ddPCR, predicted early relapse [6].
Enabling efficiency
Highly sensitive assays with rapid turnaround times allow researchers to detect drug-resistant markers within cancer samples quickly. Although MRD signals are subtle, innovative technologies can provide the ultrasensitive detection that researchers need to rapidly detect and analyse changes in ctDNA levels. Streamlined workflows with rapid analysis times in clinical labs have the potential to translate into enhanced decision-making in the clinic.
With the growing incidence of cancer, demand for MRD analysis is expected to increase. It’s critical we systematically meet this need with an ultrasensitive platform to maximize data collection and shorten turnaround times while reducing costs. This provides the best chance to advance health care and improve the quality of lives in patients.
Better biopsies
Liquid biopsies are now used in many cancer patients to identify mutations that could help guide treatment. With greater sensitivity, however, these tests could become useful for far more patients. Most efforts to improve the sensitivity of liquid biopsies have focused on developing new sequencing technologies to use after the blood is drawn. While brainstorming ways to make liquid biopsies more informative, scientists came up with the idea of trying to increase the amount of DNA in a patient’s bloodstream before the sample is taken. A tumour is always generating new ctDNA, and that’s the signal that we’re attempting to detect in the blood draw. Existing liquid biopsy technologies, however, are limited by the amount of material you collect in the tube of blood.
Our body uses two primary strategies to remove cell-free DNA from the bloodstream. Enzymes called DNases circulate in the blood and break down DNA that they encounter, while immune cells known as macrophages take up cell-free DNA as blood is filtered through the liver. By shielding the cell-free DNA from degradation by the nucleases that are in circulation and block macrophages from taking up these molecules, scientists expect to shift the balance to where the tumour is releasing DNA faster than is being degraded, increasing the concentration in a blood draw [7].
Cell-free mRNA expression as a MRD biomarker
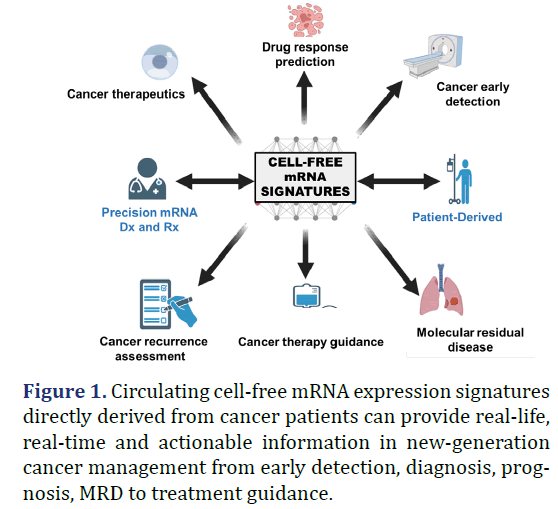
Circulating cell-free mRNA (cfmRNA) has gained attention as a potential biomarker for various diseases due to its accessibility through non-invasive methods such as blood sampling. The analysis of cfmRNA can provide valuable information about the gene expression patterns and molecular alterations associated with different physiological and pathological conditions. By profiling the cfmRNA, researchers can identify specific RNA signatures or changes in gene expression that are indicative of disease presence, progression, response to treatment or MRD [8]. cfmRNA is a dynamic and heterogeneous population of RNA molecules, originating from multiple tissues and cell types in the body. Consequently, the identification and interpretation of specific cfmRNA signatures enable researchers to explore its diagnostic, prognostic, and therapeutic potential in cancer (Figure 1).
Unlike ctDNA, which represents tumour-specific genomic alterations, cfmRNA provides insights into both tumour and non-tumour microenvironment as well as the tissue of origin. By analysing patientderived gene expression profiles within cfmRNA, it becomes possible to identify the affected tumour vulnerability, offering a non-invasive approach to inform drug efficacy [9].
In cases where tumour DNA discharge into the bloodstream is limited, cfmRNA can serve as a valuable alternative for cancer detection and monitoring, i.e., two copies vs. hundreds of copies per cell. Analysis of cfmRNA expression patterns allows for the detection of tumour-specific signatures, even at low levels, providing an opportunity for early intervention and improved patient outcomes [10].
The cfmRNA-based liquid biopsy allows for real-time monitoring of treatment response and the detection of MRD. By analysing changes in the expression levels of specific cfmRNA molecules associated with the tumour, clinicians can assess the effectiveness of treatment and detect the presence of residual disease after therapy. This information can guide treatment adjustments and greatly benefit patients.
Discussion
Liquid biopsy and NGS can detect minute numbers of cancer cells and determine whether the treatment has completely eradicated the cancer. MRD detected by liquid biopsy can also be used to track the efficacy of treatment and adjust the therapy the patient is receiving. Compared to tissue biopsy, liquid biopsy is less invasive and therefore can be performed repeatedly over time to get a longitudinal view of cancer progression. MRD has emerged as one of the most important predictors of patient outcome and clinical trial endpoint in cancer. The residual disease present after chemotherapy can lead to patient relapse, so by measuring MRD, clinicians can stratify patients into low- and high-risk groups to guide treatment.
There is an unfulfilled clinical need to better determine who benefits from adjuvant treatment after surgical resection. The tumour-informed whole genome sequencing-based approach can track thousands of tumour-specific mutations in cell-free DNA, thereby offering a highly sensitive and specific ctDNA MRD solution. Combined with the relatively short turnaround time, which meets the timelines for clinical decision-making, ctDNA-guided treatment de-escalation is now within reach.
Circulating cfmRNA carries valuable information about gene expression, alternative splicing, posttranscriptional modifications, and other RNA-based processes. This comprehensive molecular profiling provides a dynamic snapshot of the molecular landscape of disease. As RNA expression patterns can change over time, cfmRNA-based liquid biopsy allows for the monitoring of disease progression, response to treatment, and the emergence of treatment resistance. This dynamic profiling can inform clinical decision-making and enable the timely adjustment of personalized treatment strategies.
The cfmRNA-based liquid biopsy can be combined with other liquid biopsy approaches, such as ctDNA and Circulating Tumour Cell (CTC) analysis, to provide a more comprehensive view of a patient’s disease status. Integrating multiple biomarkers from different sources can enhance sensitivity, specificity, and overall MRD testing accuracy.
Conclusion
As MRD plays an ever more important role in guiding therapy in cancer patients, a standardized assay will ensure accurate and reproducible results in clinical practice and across future multicentre trials. As mounting evidence demonstrates its prognostic value, the use of MRD testing will continue to increase. However, highly sensitive tools must be employed to take full advantage of this technique and deliver maximum value in patient care.
References
- Drandi D, Alcantara M, Benmaad I, Söhlbrandt A, Lhermitte L, Zaccaria G, et al. Droplet digital PCR quantification of mantle cell lymphoma follow-up samples from four prospective trials of the European MCL Network. Hemasphere 2020;4(2):e347.
[Crossref] [Google Scholar] [PubMed].
- Yu HA, Schoenfeld AJ, Makhnin A, Kim R, Rizvi H, Tsui D, et al. Effect of osimertinib and bevacizumab on progression-free survival for patients with metastatic EGFR-mutant lung cancers: A phase 1/2 single-group open-label trial. JAMA Oncol 2020;6(7):1048-1054.
[Crossref] [Google Scholar] [PubMed]
- Chin RI, Chen K, Usmani A, Chua C, Harris PK, Binkley MS, et al. Detection of solid tumor Molecular Residual Disease (MRD) using circulating tumor DNA (ctDNA). Mol Diagn Ther 2019;23(3):311-331.
[Crossref] [Google Scholar] [PubMed]
- Tsao SCH, Weiss J, Hudson C, Christophi C, Cebon J, Behren A, et al. Monitoring response to therapy in melanoma by quantifying circulating tumor DNA with droplet digital PCR for BRAF and NRAS mutations. Sci Rep 2015;5:11198.
[Crossref] [Google Scholar] [PubMed]
- Atallah E, Schiffer CA, Weinfurt KP, Zhang MJ, Radich JP, Oehler VG, et al. Design and rationale for the Life After Stopping Tyrosine kinase inhibitors (LAST) study, a prospective, single-group longitudinal study in patients with chronic myeloid leukemia. BMC Cancer 2018;18(1):359.
[Crossref] [Google Scholar] [PubMed]
- Tarazona N, Gimeno-Valiente F, Gambardella V, Zuñiga S, Rentero-Garrido P, Huerta M, et al. Targeted next-generation sequencing of circulating-tumor DNA for tracking minimal residual disease in localized colon cancer. Ann Oncol 2019;30(11):1804-1812.
[Crossref] [Google Scholar] [PubMed]
- Martin-Alonso C, Tabrizi S, Xiong K, Blewett T, Sridhar S, Crnjac A, et al. Priming agents transiently reduce the clearance of cell-free DNA to improve liquid biopsies. Science 2024;383(6680):eadf2341.
[Crossref] [Google Scholar] [PubMed]
- Yeh JS, Lin ST. Minimal residual disease in solid tumors: Shifting the focus from cell-free DNA to cell-free RNA. J Oncogenomics and Oncotarget 2022;1:1-9.
- Yeh C, Lin ST, Lai HC. A transformative technology linking patient’s mRNA expression profile to anticancer drug efficacy. Onco 2024;4(3):143-162.
- Yeh C. Circulating cell-free transcriptomics in cancer. J Lung Pulm Respir Res 2023;10(2):27‒29.